Why Choose Tibial Interlocking Nail for Fracture Repair?
The choice of a Tibial Interlocking Nail for fracture repair is increasingly supported by clinical evidence. Recent studies suggest that this method provides superior stability compared to traditional techniques. For instance, the Journal of Orthopaedic Trauma published data showing an 85% success rate in tibial fracture union with interlocking nails. This is a significant improvement over older methods, which report lower union rates.
Patients appreciate the minimal invasiveness of the Tibial Interlocking Nail. This approach often leads to shorter recovery times and less postoperative pain. However, it is essential to recognize that not every case is ideal for this intervention. Complications can arise, including infection or misalignment. Surgeons must carefully assess each patient's situation.
The Tibial Interlocking Nail represents a robust option in orthopedic surgery. Yet, continuous monitoring of patient outcomes is crucial. As practitioners, we should remain vigilant and open to adapt our techniques based on patient feedback and evolving data. This commitment to improvement helps enhance surgical practices and patient satisfaction in the long run.
Benefits of Tibial Interlocking Nail in Fracture Management
Tibial interlocking nails are a powerful tool in fracture management. They provide stable fixation for complex tibial fractures. This method allows for early mobility in patients. Achieving better alignment is crucial for recovery. Surgeons find this method beneficial for its biomechanical advantages.
One key highlight is the reduced risk of malunion. Controls for rotation and angulation can greatly impact healing. Additionally, these nails can often be inserted without extensive exposure. This minimally invasive approach helps in faster recovery. Patients usually experience less soft tissue damage. However, some doctors may struggle with the technique and require more practice.
Despite the many benefits, complications can still arise. Infections at the nail site are a concern. Long-term outcomes can be mixed, depending on patient factors. It’s vital for both patients and surgeons to weigh the pros and cons. Continuous reflection on technique is needed for improvement. Each case presents unique challenges and nuances.
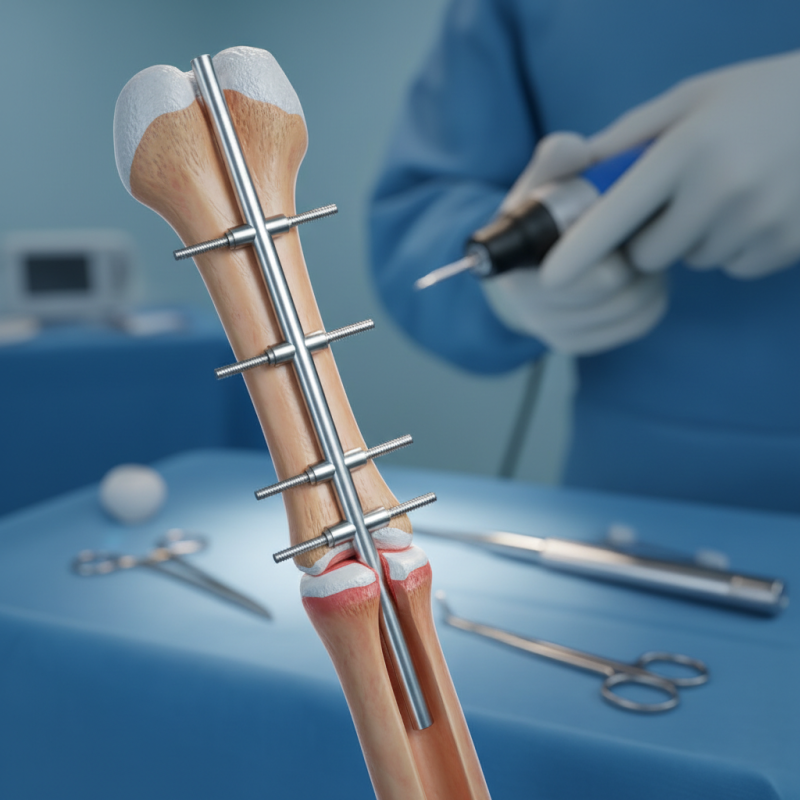
Mechanism of Action: How Tibial Interlocking Nails Work
Tibial interlocking nails are popular for treating fractures. They provide strong stabilization during the healing process. The device is inserted into the medullary canal of the tibia. This offers internal support to the fractured bone. The nails have holes that allow screws to be placed in different angles. This locking mechanism prevents the nail from moving, which is crucial for recovery.
When applied correctly, the nails distribute weight evenly across the bone. This helps in reducing complications during the healing phase. The design allows for better alignment and stabilization of fractured segments. Surgeons appreciate the flexibility these nails provide in complex fracture cases. However, it is vital to consider individual patient conditions before opting for this method.
Tip: Always consult with a specialist to understand the best approach for your specific injury. Each case can differ greatly, and what works for one might not work for another. Healing requires patience, and unexpected issues can arise. Listening to your body and following medical advice is key.
Comparison with Alternative Fracture Repair Techniques
Tibial interlocking nails are increasingly preferred for fracture repair. They provide stable support for the healing bone. This technique can be less invasive than some traditional methods. However, it isn't always the best choice for every patient.
Alternative techniques include external fixation and plate fixation. External fixators are useful for complex fractures. They allow for easy access to the fracture site. Nonetheless, they can be uncomfortable and prone to infection. Plate fixation requires a larger incision. It can offer strong stability but may involve longer recovery times.
Each method has its limitations. Tibial interlocking nails can sometimes lead to complications such as malalignment. Patients may experience pain at insertion sites as well. Understanding the pros and cons of each technique is vital. A thorough discussion with healthcare providers is essential for choosing the best approach.
Postoperative Outcomes and Recovery with Tibial Interlocking Nails
Postoperative outcomes with tibial interlocking nails show promising results. Patients often experience improved stability during recovery. The interlocking design minimizes the risk of malalignment, which is crucial for proper healing. Many individuals regain mobility faster than with traditional methods. However, some patients may face complications. These can include infection or delayed union. Such issues remind us that every procedure carries risks.
Recovery timelines can vary widely. Some patients report weight-bearing status in a few weeks, while others take longer. Pain management is another critical aspect. While many find relief with standard measures, a few still struggle with persistent discomfort. Monitoring for potential issues is essential in these cases. Regular follow-ups help catch problems early.
Additionally, the emotional toll cannot be ignored. The journey to recovery often involves mental challenges. Frustration may arise if progress is slow. Support systems play a vital role. Family and friends can provide encouragement during tough times. Yet, patients need to remain patient with their healing processes. Each body is unique, and healing takes time.
Indications and Contraindications for Using Tibial Interlocking Nails
Tibial interlocking nails are an effective option for treating certain fractures. They are typically indicated for unstable tibial shaft fractures. This includes fractures that result from high-energy trauma or those with significant displacement. For patients with multiple fractures or poor bone quality, these nails provide additional stability. The interlocking feature helps to prevent rotational movements, promoting better healing.
However, not all fractures are suitable for this treatment. Contraindications include open fractures that have been contaminated. If there's severe soft tissue injury, a different approach may be necessary. Patients with infections near the fracture site should avoid this method. Additionally, individuals with certain medical conditions may not tolerate this procedure well. It’s essential to evaluate each patient's overall health before proceeding.
When considering tibial interlocking nails, reflection is vital. Every case presents unique challenges. Surgeons should weigh the benefits against potential complications. It’s a balance between ensuring stability and minimizing risks. A thoughtful approach will guide the best decision for each patient.






